Medicus curat, natura sanat
Services
Diseases
-
Glaucoma is the second leading cause of blindness. It refers to a group of diseases characterized by damage to the optic nerve associated with visual field impairments.
The most common form of glaucoma, primary open-angle glaucoma, develops gradually without alarming symptoms. Most people are unaware of any eye problem until their vision has been significantly compromised. When the optic nerve begins to suffer damage, so-called "blind spots" appear in the visual field, most often in its peripheral parts. If left untreated, glaucoma can lead to complete blindness in both eyes.
Fortunately, if diagnosed and treated early, it is possible to prevent the loss of visual functions. However, having glaucoma means regular monitoring and treatment for the rest of your life.
Clinical Signs and Symptoms:
Primary open-angle glaucoma progresses with few or no symptoms until it reaches an advanced stage. Open-angle glaucoma affects both eyes, though asymmetrically, which is why the loss of vision in one eye is often noticed first.
Acute angle-closure glaucoma develops suddenly in response to a rapid increase in intraocular pressure, known as a glaucoma attack. On the day of the glaucoma attack, irreversible vision loss can occur, requiring immediate medical attention. Glaucoma attacks often begin in the evening or in a dimly lit room when the light is low and the pupils are relatively wide.
Symptoms include:
Blurred vision
Colored circles around lights
Redness of the eye
Severe eye pain
Nausea and vomiting
-
A cataract refers to the clouding of a person’s natural lens. Located behind the pupil, the lens functions to focus and deliver a clear image of objects at various distances in front of the eye. Clouding of the lens leads to the scattering of light, blurring of images, and a gradual decrease in vision.
What causes cataracts?
The most common cause of cataracts is aging. Factors that can trigger the development of cataracts at a younger age include eye inflammation, diabetes, UV rays, and heredity.
Treatment of Cataracts
Currently, there is no proven treatment for cataracts with drops or tablets. The only treatment for this condition is surgical.
When is Cataract Surgery Needed?
Surgery is advised when the patient struggles to see clearly things like the television, cars, and pedestrians, experiences glare during night driving, and cannot read.
What Does the Surgery Involve?
The surgery is performed using a bloodless and sutureless technique. With the help of ultrasound, through a 2.75 mm corneal tunnel, the clouded lens is extracted. An artificial lens is then implanted in its place. Using this surgical method, the patient can watch television, drive, or read as early as the next day after the operation.
-
Macular degeneration refers to the damage of the part of the eye known as the macula. This small area in the center of the retina allows us to see details in our surrounding world clearly. Macular degeneration develops as part of the natural aging process of the body. It is characterized by a wide range of clinical and pathological changes, including pale-yellow deposits called drusen, disturbances in the retinal pigment epithelium, choroidal neovascularization, and disciform macular degeneration.
Symptoms:
If you have macular degeneration, you may experience blurred vision, dark spots in the center of your vision, and difficulty seeing both up close and at a distance. Activities such as threading a needle, reading, writing, drawing, and others can be greatly impaired or even impossible.
Forms of Macular Degeneration:
The disease manifests in two forms: non-exudative (dry) and exudative (wet or neovascular).
Drusen are typical changes for the dry form, while neovascularization is typical for the wet form. Disciform macular degeneration represents the fibrotic stage of the neovascular form.
The dry form of macular degeneration is more common, affecting 90% of people with this condition. Vision loss occurs over a longer period compared to the wet form. The neovascular form is seen in 10% of patients with the condition, where vision loss may be more significant and occur over a shorter period. Pathologically proliferated blood vessels leak fluid or blood, leading to blurred vision, dark spots, and other complaints.
Treatment Methods:
Treatment of the dry form of macular degeneration. Treatment with antioxidants and zinc may slow the progression of the early stages of dry macular degeneration. There is no known treatment to prevent vision loss in advanced stages of this form of macular degeneration.
Treatment of the wet form of macular degeneration includes:
Laser photocoagulation
Photodynamic therapy with Visudyne
Intravitreal injection of medications targeted against VEGF (vascular endothelial growth factor)
It is important to note that none of these methods can completely cure the disease and that it may progress despite treatment.
Regular follow-up examinations with your ophthalmologist are necessary.
-
Dry eye syndrome is a condition associated with reduced tear production or accelerated evaporation of tears, or an imbalance in the components of the tear film. Dry eye can result from systemic diseases as well as purely ocular pathology.
What causes it?
Advanced age
Menopause
Contraceptives
Systemic autoimmune diseases
Use of a wide range of medications
Hypovitaminosis
Eye injuries
Burns
Use of contact lenses
Inflammation of the conjunctiva and cornea
Neurological disorders, and others.
Treatment Methods
The methods vary depending on the severity of the condition: use of artificial tears, gels, moisturizing chambers. In the most severe cases, synthetic plugs are implanted in the tear ducts to preserve the small amount of naturally produced tears.
Therapies and Procedures
-
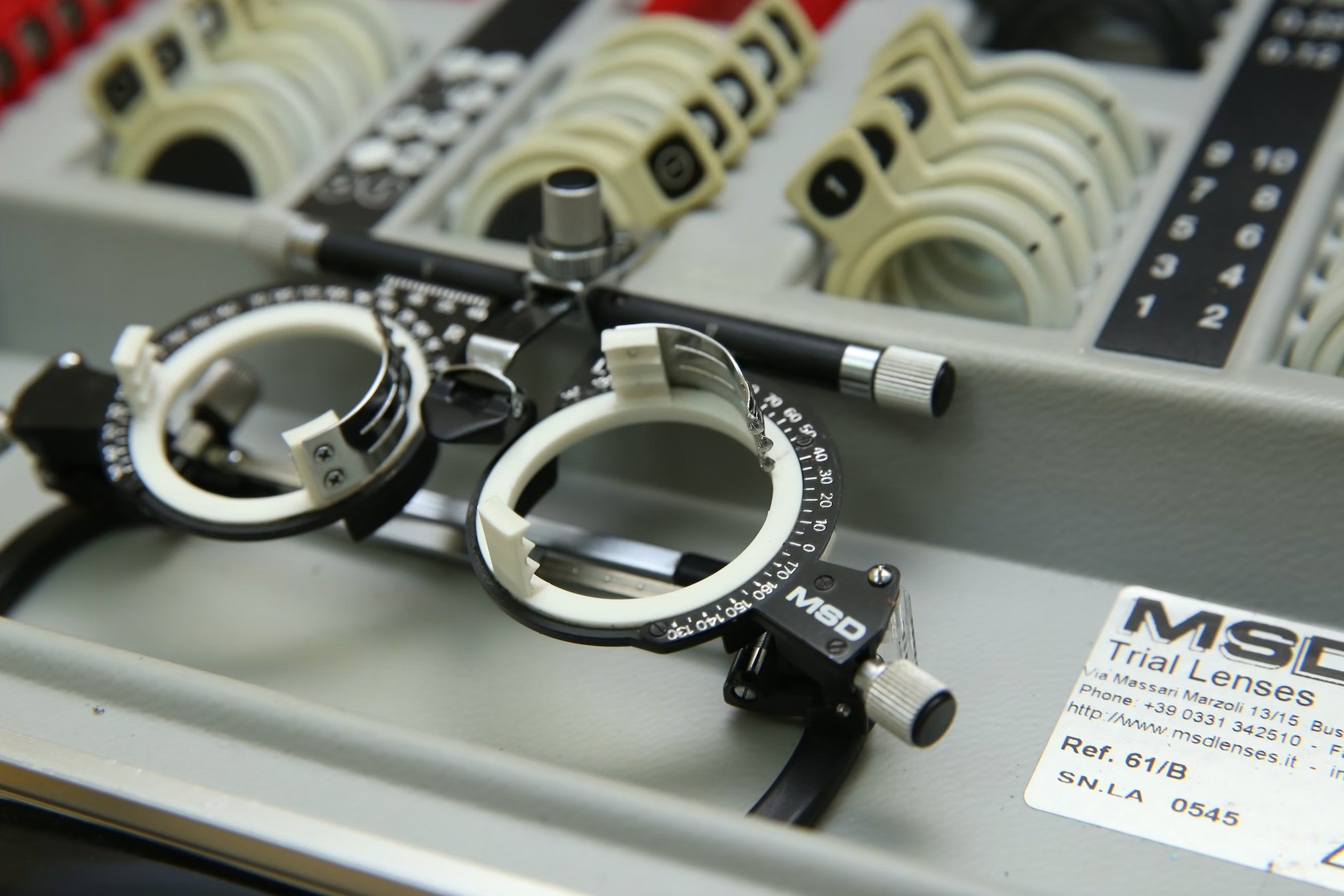
What is the test?
Tonometry is a method for indirectly measuring intraocular pressure, specifically assessing the eye's ability to deform.
When is it conducted?
Tonometry is primarily performed to diagnose glaucoma (an eye disease accompanied by increased intraocular pressure) and many other diseases associated with increases or decreases in intraocular pressure (such as retinal detachment, etc.).
How is it conducted?
There are two main methods: Non-contact (air puff) tonometry, where the patient's eye is not touched; Contact tonometry involves applying a drop of anesthetic to the front surface of the eye, then touching it with a fine instrument to measure the pressure.
The instrumental examination provides accurate information about the pressure:
Impression tonometry (based on pressing against the front surface of the eye towards the center of the eyeball);
Applanation tonometry (measures the eye's ability to flatten when in contact with the surface of the tonometer, and the printout (tonogram) is analyzed).
-
This is a method for examining the visual field.
The visual field is that part of space that we perceive when looking at a specific fixation point.
The examination is particularly important in the diagnosis and monitoring of glaucoma, as well as diseases affecting the visual pathways.
-
Optical Coherence Tomography is an imaging method for viewing the structures of the retina. An infrared laser beam scans the area under examination and constructs an image of the structures in depth with near-microscopic precision.
This method is used for early diagnosis of glaucoma and retinal diseases.




